A Surgeon’s Guide to Septoplasty: Before, During and After

Do you find yourself constantly shifting positions at night because you can only breathe through one nostril?
Does your partner complain about your snoring or loud breathing while you sleep? Or maybe your mouth is dry because you can’t breathe through your nose.
If this describes you, then you might have a deviated septum, or be considering septoplasty.
Let’s take a look at what a deviated septum is, how septoplasty surgery can help you, and what to expect if you decide to get septoplasty.
What Is a Deviated Septum?
The nasal septum is a wall of cartilage and bone that separates the nose into two distinct halves. Your nostrils can then effectively channel the air you breathe up through your nose.
The nasal septum should be fairly straight, but it can become crooked, deviating to one side or the other. This is called a deviated septum.
A deviated septum constricts at least one side of the nose, keeping air from flowing freely.
Causes of a Deviated Septum
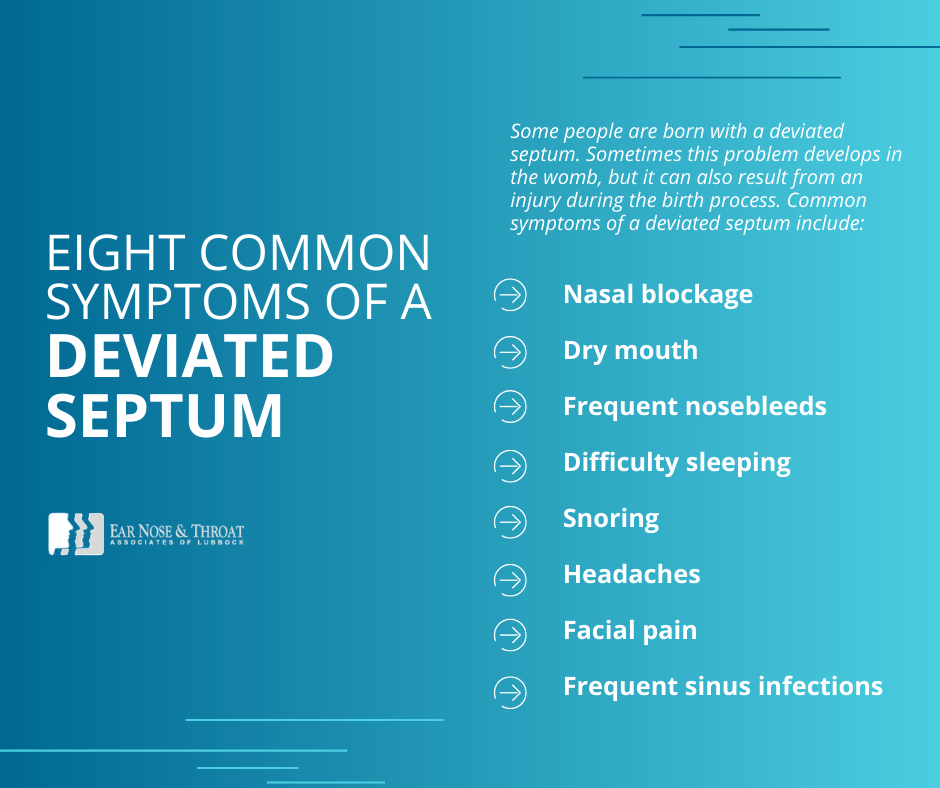
Some people are born with a deviated septum. Sometimes this problem develops in the womb, but it can also result from an injury during the birth process.
Injuries to the nose can also cause a deviated septum. Common sources of such trauma include car accidents, sports injuries, and hits to the face during fights. Even if the nose doesn’t break, a deviated septum can still occur.
Symptoms of a Deviated Septum
When the nasal septum becomes crooked, it can restrict the airflow through one or both sides of the nose. This blockage is often constant because it isn’t caused by allergies or a cold, but a physical obstruction.
A nasal blockage, especially on both sides of the nose, forces you to breathe through your mouth. This mouth breathing can cause a dry mouth. Your nose may dry out as well, leading to frequent nosebleeds.
The obstruction to your breathing can also cause snoring as well as difficulty sleeping. If you also have sleep apnea, your snoring may be severe, and you may have trouble using your CPAP machine.
Other symptoms of a deviated septum can include headaches, facial pain and frequent sinus infections.
What Is Septoplasty?
Septoplasty is a corrective surgery to straighten the nasal septum without needing to remove much (if any) cartilage or bone. It can be performed under general or local anesthesia, depending on the degree of deviation.
The surgeon makes a small incision inside the nose. This incision allows the surgeon to straighten the nasal septum, which improves nasal airflow.
Before Your Septoplasty Surgery
Preparing for a septoplasty is similar to preparing for most other surgical procedures that involve general anesthesia.
We ask you to refrain from eating and drinking after midnight the night before your procedure. This helps reduce your chance of aspirating anything from your stomach during anesthesia.
Be sure to tell your surgeon if you take any blood thinners. You may be instructed to stop taking these before your septoplasty.
You should also shower with antibacterial soap before your procedure.
If you would like to trim your nose hair beforehand, feel free to do so. But there isn’t much you need to do to prepare for a septoplasty surgery. We wouldn’t even ask you to trim your hard-earned mustache!
The Day of Your Septoplasty Surgery
If your nasal septum is only mildly deviated, the ENT surgeon might be able to correct it in an office procedure with local anesthesia! But most of the time, especially for severe deviations, septoplasties are performed under general anesthesia at a surgery center.
Upon your arrival at the surgery center, a nurse will place an IV catheter in your arm. After you talk with your surgeon, the anesthesiologist, and the nurse, you will be given general anesthesia.
The septoplasty itself is relatively simple and painless. The procedure usually takes between 30 and 60 minutes to perform. You can expect to wake up from surgery with plastic splints in your nose (which hold the septum straight while it heals), and perhaps dissolvable packing material.
The splints and packing will make it very difficult to breathe through your nose for several days, so patients should not expect immediate relief following surgery.
Septoplasty is usually an outpatient surgery, so you will be released to go home the same day.
After Your Septoplasty Surgery
Following a septoplasty, you should expect moderate nasal congestion while your nose heals. It is very important to use saline spray to keep the nose moist. This will reduce crusting and encourage the packing material to dissolve more quickly. You should use saline spray at least several times per day, or more if you like.
Light bleeding is normal for a day or two following surgery. However, if bleeding increases or continues for several days, your surgeon may have you try some Afrin nasal spray. This should be done sparingly at the direction of your surgeon, as Afrin can actually increase rebound congestion once you stop using it.
We recommend that you take two or three days off work after your septoplasty. You should take it easy for those first few days, but we don’t recommend staying in bed. Instead, try to move around and participate in simple (gentle) activities. After these first days, you can return to work and your normal daily routine.
The plastic splints will be removed in the doctor’s office four or five days after your surgery. Once these are removed, it will be much easier to breathe through your nose, though you may still have some packing material that has yet to dissolve.
You should continue to use your saline spray, or you can even try a saline irrigation to clear out any remaining crusting or packing. This may take another week or two to resolve, so don’t worry if you’re still congested or having some difficulty breathing through your nose a couple of weeks after surgery.
You’ll be scheduled for a final postoperative appointment about four weeks after your surgery to make sure you’re healing well and seeing good results from your procedure.
After recovering from their septoplasty surgery, many people say they can breathe more easily, sleep better and snore less.
Septoplasty surgery doesn’t correct sleep apnea, which is a different medical issue. So if you used a CPAP device for sleep apnea before your septoplasty, you will still need to use it after your surgery.
The good news is, many people find that they tolerate their CPAP machine much better after their septoplasty surgery.
Could Septoplasty Help You?
The surgeons at ENT Associates of Lubbock are experienced in performing septoplasties, along with many other surgeries. If you’ve been suffering from difficulty breathing, one-sided congestion, and snoring, reach out to us for a consultation.
If septoplasty isn’t the right procedure for you, we’ll help you find the treatment that works for your specific situation. We look forward to meeting you!
Dr. Scolaro is a board-certified Otolaryngologist servicing the South Plains area. He has been practicing in Lubbock since 1990 and has earned a reputation as a skilled and experienced surgeon. He currently serves as the Medical Director for Covenant High Plains Surgery Center campuses, is a member of Covenant Health Partners and is an adjunct faculty professor for Texas Tech University Health Sciences Center School of Medicine. Learn more about Dr. Scolaro.
Categories: