Welcoming a baby into the world is an incredible experience. But finding out your sweet new baby has a tongue tie can quickly send any parent into a whirlwind of stress and anxiety.
Fortunately, in most cases, a doctor can fix a child’s tongue tie quickly and easily with a minor procedure called a frenotomy.
If you’re considering a frenotomy for your child’s tongue tie, here’s what you need to know.
What Is a Tongue Tie and When Does It Require Treatment?
A tongue tie (also called ankyloglossia) involves a small piece of tissue called the lingual frenulum, which connects the underside of the tongue to the bottom of the mouth. A normal frenulum allows the tongue to move fairly freely, but sometimes people are born with their frenulum in a position that hinders the tongue’s range of motion, “tying” the tongue to the floor of the mouth.
To be clear, when a person has a tongue tie, there’s nothing wrong with the tongue itself. It’s simply anchored too tightly, and that anchor won’t let the tongue move up or forward like it should. You can think of it like a rope holding the tongue down. As soon as that rope is cut, the tongue is free to function normally.
Parents often notice a tongue tie when their child has trouble breastfeeding or learning to speak clearly. A doctor can diagnose a tongue tie with a physical exam, but depending on the severity, it may or may not require surgical treatment.
If you know or suspect your child has a tongue tie, you may wonder whether they need surgical intervention. Generally speaking, here’s the rule of thumb we follow:
- If a person can extend their tongue about five millimeters past their teeth and the condition doesn’t cause any issues with function, we don’t recommend surgery.
- If the tongue tie is more severe and interferes with necessary oral functions, we recommend correcting it surgically with a frenotomy.
What Is a Frenotomy?
A frenotomy is a simple surgical cut that releases the tongue, allowing it to move freely.
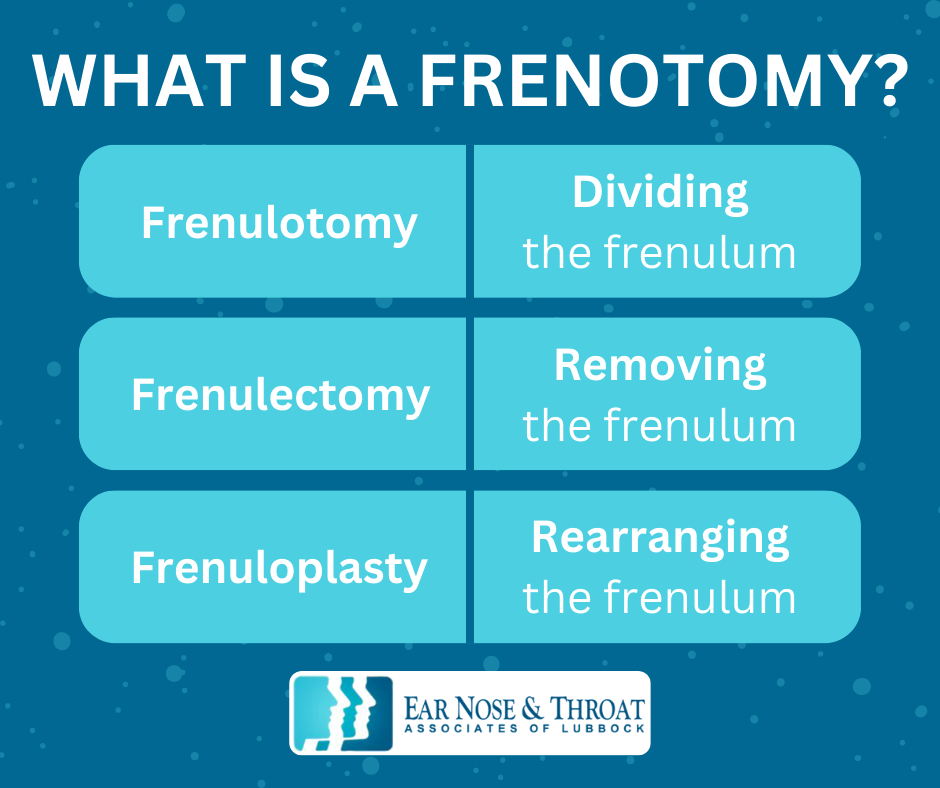
It’s also sometimes called a frenulotomy, frenulectomy, or frenuloplasty, all Latin terms that refer to very similar things:
- Frenulotomy means dividing the frenulum.
- Frenulectomy means removing the frenulum.
- Frenuloplasty means rearranging the frenulum.
During a frenotomy, we use sterile scissors to gently snip the frenulum under the tongue. Since the tissue has minimal nerves and blood flow, it barely bleeds, and the patient feels minimal discomfort.
Although it might be difficult to imagine your baby or young child undergoing any surgical procedure, it really is quick and simple. In fact, it’s a lot like getting their ears pierced! It’s over within seconds and doesn’t require anesthesia — just holding their head still for a few moments.
Afterward, you can immediately nurse your child to help calm and comfort them. Older children can have a drink right away.
Can a Doctor Complete a Frenotomy In-Office?
We typically perform frenotomies in the office. Newborns and infants tolerate a frenotomy very well, and we can easily hold them still for the few moments it takes to safely snip the frenulum.
A five-year-old may not be as cooperative. If a child isn’t able to sit still for the procedure, it could be dangerous for us to attempt it. In these cases, we can administer lidocaine to numb the area and help calm the child, ensuring their safety.
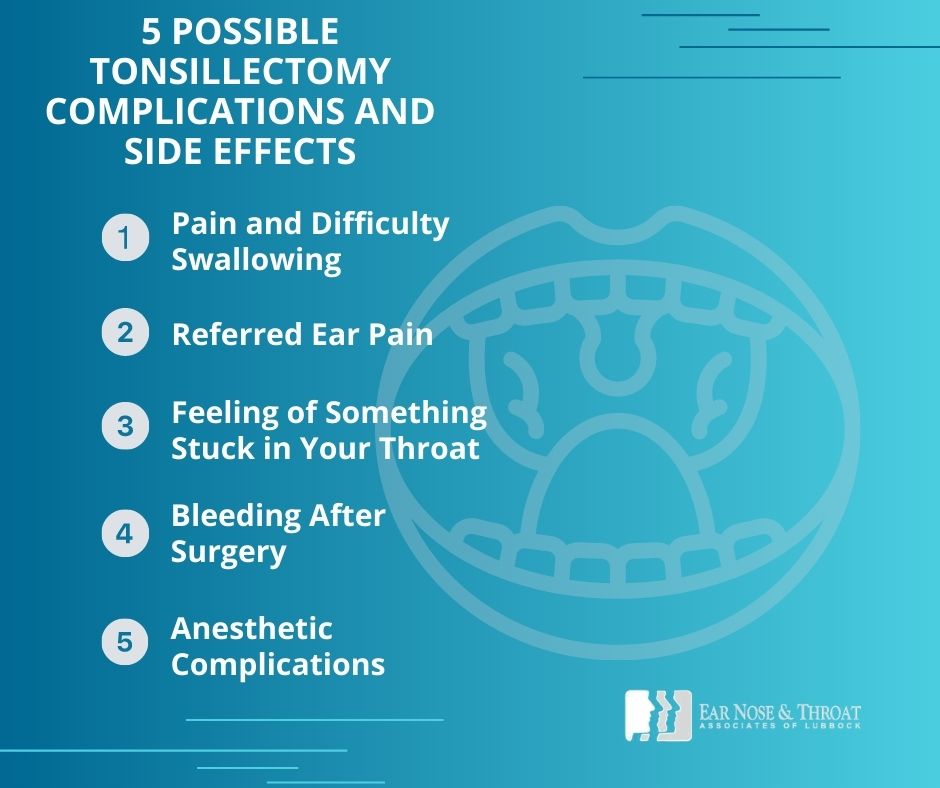
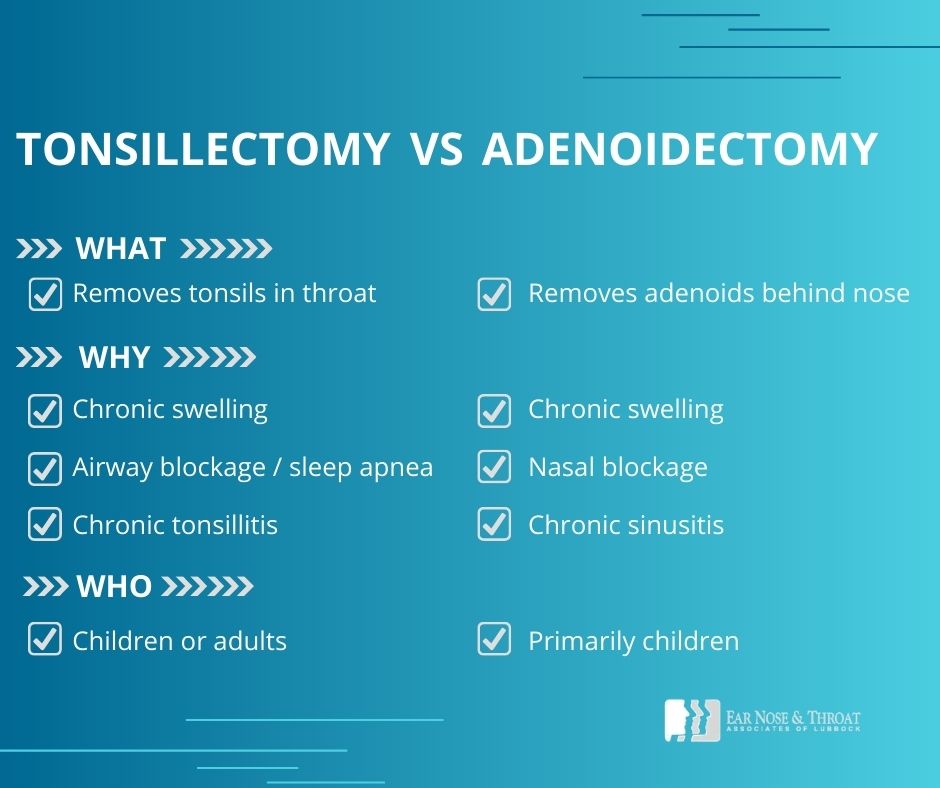
If a patient is already scheduled for another surgical procedure, like a tympanoplasty (ear tube placement) or tonsillectomy (tonsil removal), we can complete the frenotomy at the same time in the operating room while they’re under anesthesia.
What About an Upper Lip Frenulectomy?
The lingual frenulum isn’t the only frenulum of the body. Another frenulum sits where the center of your upper lip meets your gum. (If you lift your tongue above your front two teeth, you can feel the small, stretchy band of tissue there.)
When this tissue attaches to the upper lip in a way that limits movement or interferes with the teeth, it’s called an upper lip tie.
Unlike a tongue tie, an upper lip tie doesn’t usually cause problems with oral functions like swallowing or speaking. Since a labial (lip) frenulectomy — the surgery to fix an upper lip tie — is more complex than a lingual (tongue) frenotomy, involving more bleeding and a less certain outcome, treatment isn’t necessary or helpful in the absence of symptoms.
In some cases, however, a very large upper lip tie can interfere with nursing or cause unwanted spacing or cosmetic issues between the upper front teeth.
Because properly correcting an upper lip tie involves raising a mucosal flap and removing some tissue between the teeth, we recommend seeing an experienced oral surgeon or pediatric dentist for assessment and treatment. They have specific medical expertise in these oral structures and offer the best path toward a successful outcome.
Early Intervention Is Key
A tongue tie often comes to light when a lactation consultant or speech therapist identifies it as the source of a child’s nursing or speech problems. If you or your child’s specialist notice a possible tongue, we recommend consulting your pediatrician and/or ENT as early as possible. Tongue ties can interfere with feeding and impact a child’s oral functions as they grow and develop, so it’s a good idea to get them assessed and treated promptly.
When all is said and done, a frenotomy is a simple and effective solution to tongue ties, and nothing to be worried about. It’s quick, it’s easy, and it gives your child perfectly normal tongue function without any long-term consequences.
Dr. Scolaro is a board-certified Otolaryngologist servicing the South Plains area. He has been practicing in Lubbock since 1990 and has earned a reputation as a skilled and experienced surgeon. He currently serves as the Medical Director for Covenant High Plains Surgery Center campuses, is a member of Covenant Health Partners and is an adjunct faculty professor for Texas Tech University Health Sciences Center School of Medicine. Learn more about Dr. Scolaro.