Are Your Symptoms Just Allergies, or Do You Need a Doctor?

When you suffer with chronic allergies, you get used to many of the symptoms.
Itchy, watery eyes? You know the drill. Sneezing through every West Texas dirt storm? It’s old hat to you.
But every once in a while, a new symptom makes an appearance, and you’re left scratching your head (and not just your nose).
Can allergies give you a fever? Can allergies cause shortness of breath? Can allergies cause headaches? Do these symptoms mean you need to call a doctor, or is it just another part of the fun of fighting seasonal allergies?
We’ll explore all of this and more.
What Symptoms Can Allergies Cause?
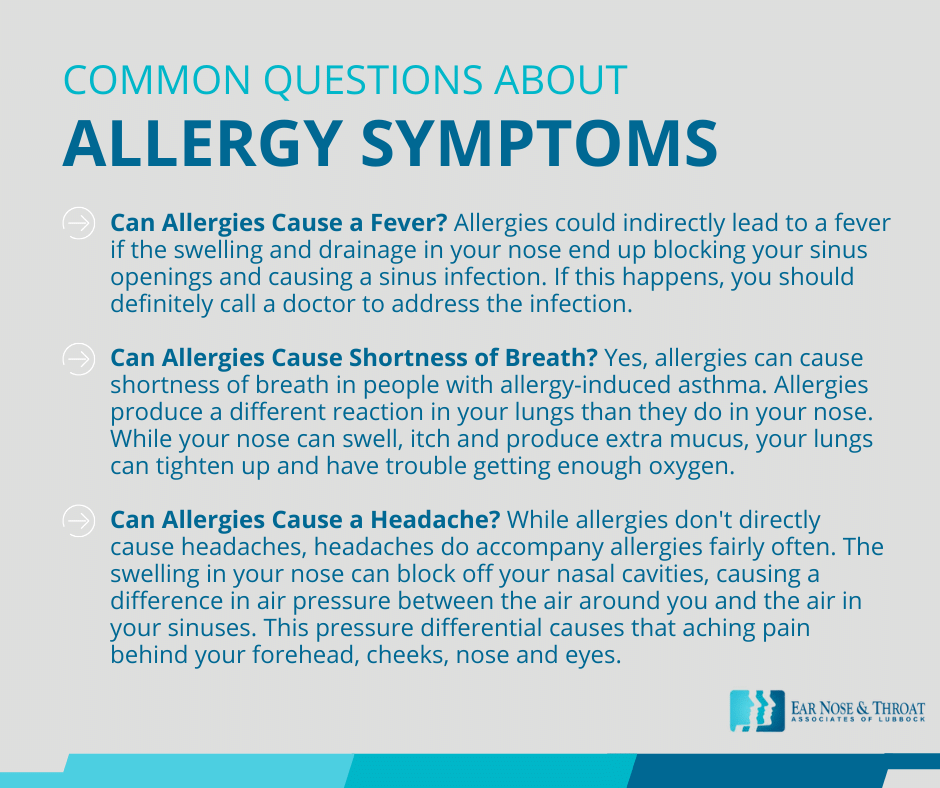
Can Allergies Cause a Fever?
Despite the commonly used term “hay fever,” allergies in and of themselves don’t cause a fever.
Respiratory allergies are really just an overreaction of your immune system to particles in the air. Your immune system’s job is to fight off viruses and bacteria in your environment and keep them from causing an infection. But sometimes your immune system perceives a piece of pollen or dust in the air as a harmful invader, a pathogen that needs to be fought.
Your immune system produces antibodies to destroy the invaders, leading to the runny nose, sneezing and watery eyes we all know so well. But since there’s no actual infection, there’s also no fever.
Allergies could indirectly lead to a fever if the swelling and drainage in your nose end up blocking your sinus openings and causing a sinus infection. If this happens, you should definitely call a doctor to address the infection.
Can Allergies Cause Shortness of Breath?
Yes, allergies can cause shortness of breath in people with allergy-induced asthma.
Allergies produce a different reaction in your lungs than they do in your nose. While your nose can swell, itch and produce extra mucus, your lungs can tighten up and have trouble getting enough oxygen.
Some people have asthma year round, with allergies worsening at certain times of year, and some people only have asthma during allergy season.
If you experience allergy-induced asthma, then in addition to dealing with your nasal allergy symptoms you’ll also need a prescription inhaler for your lungs.
Signs of asthma include a persistent dry cough, shortness of breath, and wheezing. If you’re experiencing any of these, then you should check in with your doctor about your symptoms.
Can Allergies Cause a Headache?
While allergies don’t directly cause headaches, headaches do accompany allergies fairly often. The swelling in your nose can block off your nasal cavities, causing a difference in air pressure between the air around you and the air in your sinuses. This pressure differential causes that aching pain behind your forehead, cheeks, nose and eyes.
Some people with very narrow sinus passageways can even tell when a cold front is coming in, just like people with a weather-wise ache in a knee or hip!
An occasional headache that resolves quickly probably doesn’t warrant a call to your doctor. But if your headaches become debilitating or persists long enough to interfere with your life, know that an ENT physician can help.
Allergy Treatments for Symptom Control
Allergy symptoms are uncomfortable and can really begin to interfere with your daily activities. Fortunately, there are a variety of treatments you can try at home before you reach out to a doctor.
What Allergy Medications Should You Use?
You can find a host of over-the-counter allergy medications available at your local drugstore.
The most common class of allergy medication is the antihistamine. First-generation antihistamines like Benadryl (diphenhydramine) typically cause drowsiness. Second-generation formulations are non-drowsy and interact with fewer drugs. These include medications like Claritin (loratadine), Zyrtec (cetirizine), Allegra (fexofenadine) and Xyzal (levocetirizine).
Another class of drugs that can help deal with allergy symptoms is the mucolytic, which breaks up mucus and allows the body to clear congestion more easily. Mucinex (guaifenesin) is a good example of a mucolytic.
Topical steroids for allergies include nasal sprays such as Flonase (fluticasone), Rhinocort (budesonide) and Nasonex (mometasone). They are generally well tolerated and work to reduce allergy symptoms like runny nose, swelling and inflammation. However, they do have some fairly common side effects like headaches and nosebleeds.
Finally, you can try using a neti pot or other saline irrigation system to rinse out the nose and sinuses.
What Allergy Medications Should You Avoid Long Term?
Oral decongestants like Sudafed (pseudoephedrine) and topical decongestants like Afrin (oxymetazoline) are great for treating the stuffy nose and sinus pressure of allergies in the short term. However, decongestants should not be used on a long-term basis.
If used for more than a few days, decongestant sprays can cause rebound congestion, actually resulting in worse stuffiness than before! And decongestants in general can be dangerous for people with a history of cardiac problems, increasing blood pressure and interfering with blood pressure medications.
Some allergy medications have a “D” on the end of their names, meaning they include a decongestant along with the primary drug (think Claritin D, Mucinex D or Allegra D). These shouldn’t be used long term either.
Are Your Allergies Causing New or Worsening Symptoms?
If after trying the treatments mentioned above, your allergy symptoms don’t improve after a month or two, it’s helpful to know you don’t have to continue to suffer on your own. Whether your allergies cause shortness of breath, headache, runny nose or sinus infections that lead to fever, there’s help and relief available to you.
ENT doctors have the training and resources to address your allergy symptoms. Reach out to ENT Associates of Lubbock today. We’re experts in helping you get your life back from seasonal allergies!
Dr. Cuthbertson is a physician at Ear Nose & Throat Associates of Lubbock. He joined the team at ENT Lubbock from Houston, where he was chief resident of the prestigious Bobby R. Alford Department of Otolaryngology at Baylor College of Medicine. He is board certified in Otolaryngology and Head & Neck Surgery and has quickly built a reputation, not only as an extremely skilled surgeon, but as an approachable and compassionate clinician adept in the newest standards and technologies. Learn more about Dr. Cuthbertson.
Categories: