If you’ve discovered an abnormal mass in your parotid gland, your ENT may have recommended a superficial or total parotidectomy.
We’re aware that the mere mention of surgery can be distressing, but knowing what to expect can help. Below, we’ll walk through both types of procedures in detail, explaining what they are, why they’re necessary, and what you can expect during and after the surgeries.
What Is a Parotidectomy, and When Is It Necessary?
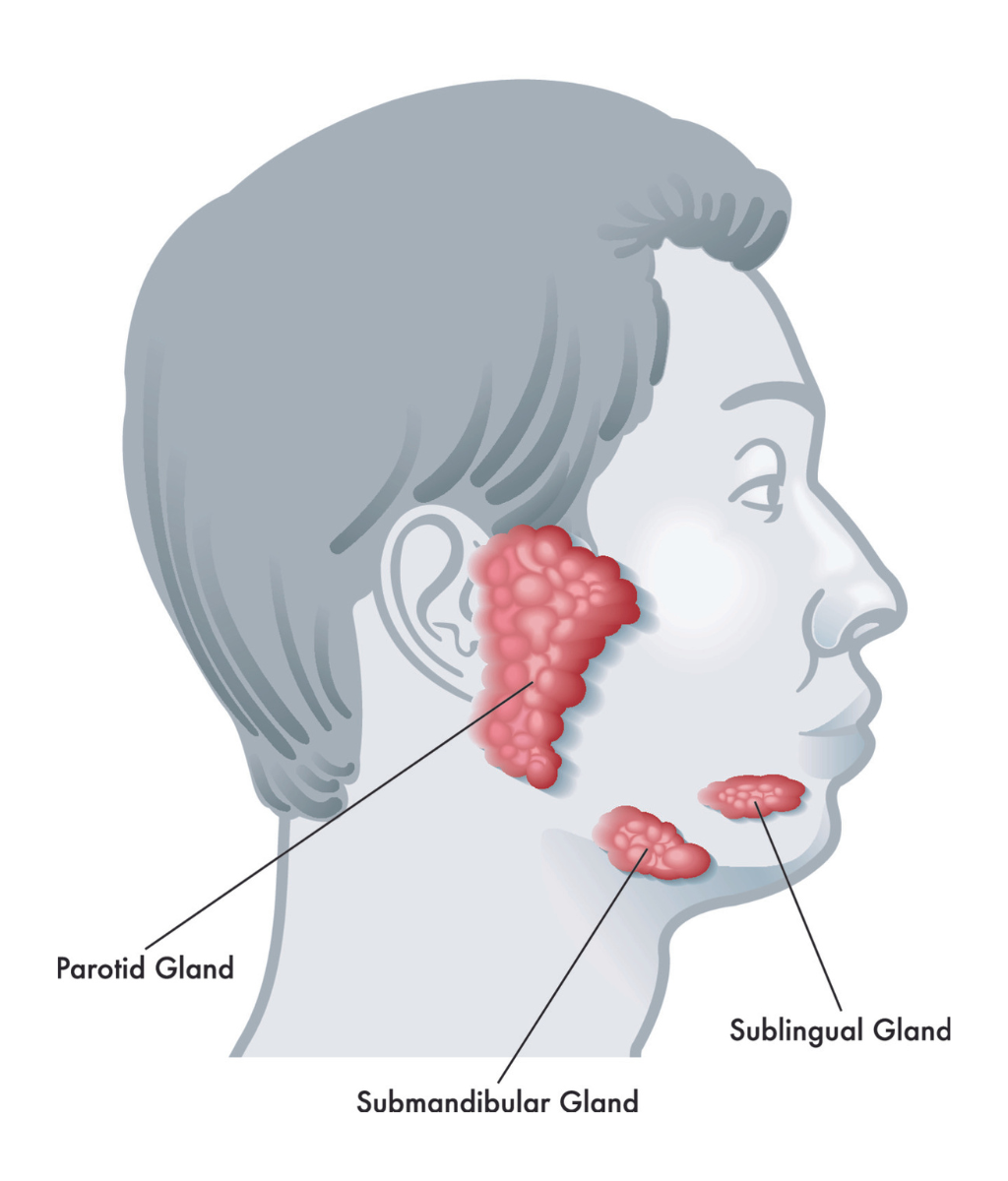
A parotidectomy is the partial or total surgical removal of the parotid gland, which sits just in front of the ear and extends down into the upper neck. The parotid gland is the largest of your major salivary glands, which produce saliva to lubricate your mouth and help with the breakdown of food.
Most of the time, ENTs recommend a parotidectomy when a patient develops a tumor in their parotid gland. About 80% of parotid tumors are benign (noncancerous), and 20% are malignant (cancerous).
Of the many kinds of benign parotid tumors, the most common is called a pleomorphic adenoma. This is an unusual type of benign tumor because, if left untreated, it can become cancerous over time. If that happens, doctors rename it a carcinoma ex pleomorphic adenoma.
Superficial Parotidectomy vs. Total Parotidectomy
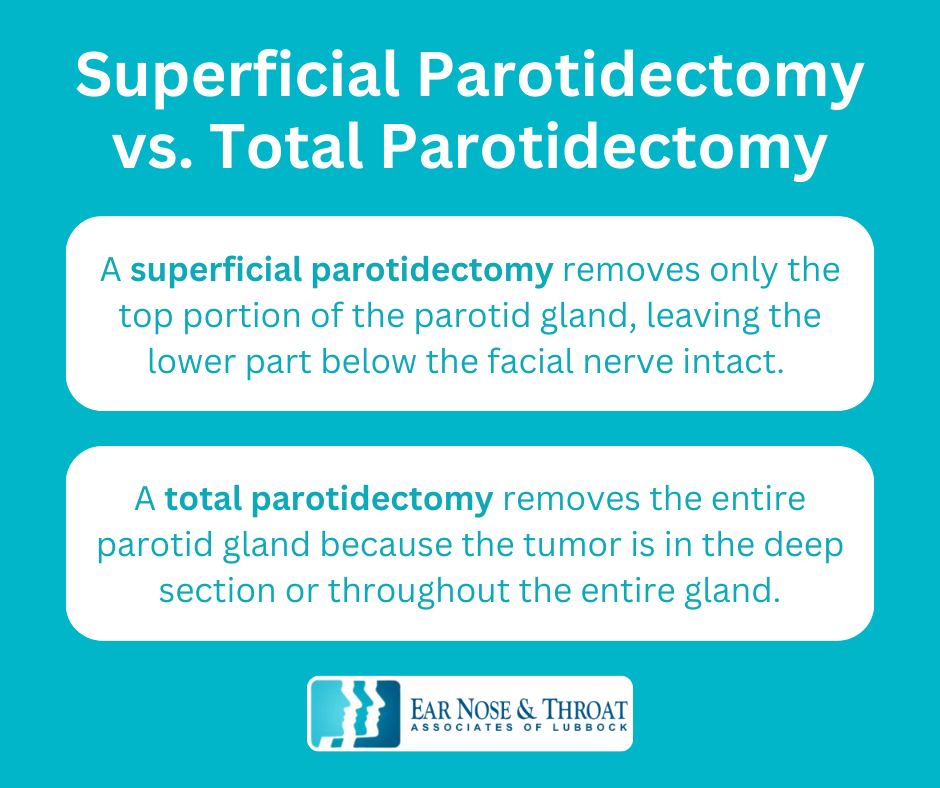
There are two types of parotidectomies: a superficial parotidectomy and a total parotidectomy.
To understand the difference between the two, it’s helpful to know a bit about the anatomy of the parotid gland.
Parotidectomies are one of the most challenging procedures ENTs perform because the facial nerve runs through the parotid gland. The facial nerve controls facial movements and expressions, so it’s very important.
About 15% of the parotid gland sits below (deeper than) the facial nerve, and 85% rests on top of (superficial to) it. The type of parotidectomy you’ll need depends on where in the parotid gland your tumor is located.
- A superficial parotidectomy removes only the top portion of the parotid gland, leaving the lower part below the facial nerve intact. Most tumors are in the top portion of the gland, so this procedure is more common.
- A total parotidectomy removes the entire parotid gland because the tumor is in the deep section or throughout the entire gland.
What to Expect During Surgery
Whether you’re having a superficial or total parotidectomy, you’ll be in a surgical center under general anesthesia.
After making an incision, we’ll carefully separate the gland from the facial nerve and its branches in order to remove the affected portion. A superficial parotidectomy involves only the top, most accessible part of the gland. A total thyroidectomy means delicately accessing and removing the portion beneath the facial nerve as well.
Once we’ve removed the affected areas of the gland, we insert a temporary drain to prevent fluid from building up in the now-empty area. We close the incision with stitches and wrap your head with bandages. You’ll come into the office the next day to have the drain removed.
What to Expect During Recovery
The recovery from either a total or superficial parotidectomy takes about a week. Because this is a more involved surgery, you may experience some lingering issues:
Facial Weakness or Paralysis
Since we’re operating so close to the facial nerve and its branches, facial weakness or paralysis is the most significant risk of a parotidectomy.
Your facial nerve has five main branches and numerous tiny offshoots spreading across your face in an intricate pattern. Each branch controls a specific area of motion or expression. If one of these branches experiences trauma during the surgery, it could temporarily or permanently lose its ability to function.
For example, after the surgery, you could experience some weakness around your eye, nose, or lower lip. The lower lip, in particular, is especially vulnerable because it has fewer nerve connections than other areas.
The most common side effect following a parotidectomy is temporary weakness in one or more facial areas, affecting as many as 20% of patients. Usually, these issues resolve on their own within six to 12 months of surgery. However, a much lower percentage of patients experience permanent weakness or paralysis.
We work as carefully as possible around your nerve network, aiming for minimal disturbance while still successfully removing the tumor. Patients needing a total parotidectomy have an increased risk of nerve damage since the surgeon must work beneath the facial nerve.
Minor Cosmetic Changes
After we remove the parotid gland, an empty space can be left behind and cause a slight depression in front of your ear. And, though the incisions from parotidectomies usually heal nicely, you may still have a visible scar in front of your ear and on your neck.
Ear Numbness
One specific nerve — the greater auricular nerve — passes through the parotid gland, which means we have to remove it in order to get the gland out. This nerve is responsible for sensation in the lower two-thirds of the ear, so patients who get a total or superficial parotidectomy experience permanent numbness in that portion of their ear. Fortunately, the loss of feeling doesn’t impact function, and most people report that they simply get used to the numbness.
Fluid Buildup
After a superficial parotidectomy, patients sometimes experience a cyst-like accumulation of salivary fluid in the area, also called a sialocele. Other times, fluid from surrounding tissues can accumulate in the space where the parotid gland used to be, creating what’s called a seroma.
We can resolve this issue by drawing the fluid out with a syringe, repeatedly if necessary. In some cases, we may make a small incision and drain the pocket of fluid that way.
Sweating After Eating (Post-Gustatory Sweating)
We know this sounds strange, so it’s good to be aware of it beforehand!
Have you ever experienced that tingling sensation in your jaw or in front of your ears after tasting something really sour, like a lemon? That’s your nerve fibers triggering your parotid gland to secrete saliva.
After we remove the gland, those nerve fibers don’t simply retire; they look for a new job. By connecting to the nearby sweat glands in your skin, the nerve fibers continue to operate when you eat — except instead of stimulating saliva production, they now stimulate a little sweat in front of your ear.
Although strange, this side effect is the least concerning of all the possible risks, and it can happen even several years after your total or superficial parotidectomy.
Coping With Preoperative Anxiety
It’s completely normal to feel nervous about having a parotidectomy, and you’re not alone if you feel anxious about what could happen during or after the procedure. However, it’s important not to let anxiety get in the way of an important — and potentially life-saving — procedure.
When a parotid tumor is cancerous, it’s often aggressive, and we need to address it as soon as possible. Even benign tumors can interfere with other facial structures and functions or become cancerous over time.
We only recommend a superficial or total parotidectomy when it’s necessary for your health and safety, and when the risks of surgery outweigh the risks of not having surgery.
Unfortunately, no one can guarantee a side-effect-free parotidectomy. However, we take many precautions to reduce your risk, including having experienced surgeons who have years of experience performing parotidectomies. Plus, addressing parotid tumors sooner rather than later can reduce the risk that they’ll grow, spread, and put more nerves at risk.
If you require a parotidectomy, we want you to know you’re in good hands. Our staff will support you throughout the process, and we’ll provide you with all the information you need to thoroughly understand your diagnosis and treatment.
Dr. Cuthbertson is a physician at Ear Nose & Throat Associates of Lubbock. He joined the team at ENT Lubbock from Houston, where he was chief resident of the prestigious Bobby R. Alford Department of Otolaryngology at Baylor College of Medicine. He is board certified in Otolaryngology and Head & Neck Surgery and has quickly built a reputation, not only as an extremely skilled surgeon, but as an approachable and compassionate clinician adept in the newest standards and technologies. Learn more about Dr. Cuthbertson.
Dr. Scolaro is a board-certified Otolaryngologist servicing the South Plains area. He has been practicing in Lubbock since 1990 and has earned a reputation as a skilled and experienced surgeon. He currently serves as the Medical Director for Covenant High Plains Surgery Center campuses, is a member of Covenant Health Partners and is an adjunct faculty professor for Texas Tech University Health Sciences Center School of Medicine. Learn more about Dr. Scolaro.