What You Need to Know About Asthma and Sleep Apnea

Did you know that if you have asthma, you also have an increased risk of developing sleep apnea, and vice versa?
Research indicates asthma and sleep apnea are indirectly connected, and each condition can potentially exacerbate the other. Although other contributing factors also play a role, knowing how asthma and sleep apnea are related and pursuing effective treatments for each may help you sleep better at night and feel well-rested throughout the day.
Let’s take a close look at each of these conditions and explore how they’re related.
How Are Asthma and Sleep Apnea Related?
Based on our professional experience and our review of recent data, we know that obstructive sleep apnea syndrome (OSAS) and asthma are indirectly connected, with each condition negatively influencing the other.
Although asthma and sleep apnea affect one another, it’s not entirely accurate to say one directly causes the other. Because there are several hypotheses out there, several factors need to be considered.
Recently, researchers have found that obstructive sleep apnea could actually be a trigger for asthma exacerbations. There are a number of different pathways as to how. It may be because OSAS causes hypoxia, or low oxygen levels in the blood and tissues. With a lack of oxygen, asthma symptoms may worsen.
Alternatively, a particular person’s airway lining could have increased irritability or a propensity for inflammation. If so, both asthma and obstructive sleep apnea may be exacerbated by that hyperactive airway lining.
What is Asthma?
Asthma is a chronic long-term condition that affects your lungs’ ability to carry air in and out. If you have asthma, your airways are overreactive and sometimes become inflamed and narrow, making breathing much more difficult.
Your entire respiratory system is split into two parts: the upper respiratory tract (your nose, mouth, and throat) and the lower respiratory tract (your lungs). When a person without asthma has an upper respiratory reaction to a trigger, their upper respiratory tract swells, causing nasal congestion and mucus production, which leads to a runny nose.
Asthma is a similar response, except that symptoms occur in the lower respiratory tract — in the lungs instead of the nose. Asthma triggers narrow the airways and makes breathing much more difficult.
Asthma exacerbations can be triggered by many things, including:
- Exercise
- Cold weather
- Pollen or other allergens
- Viral infections
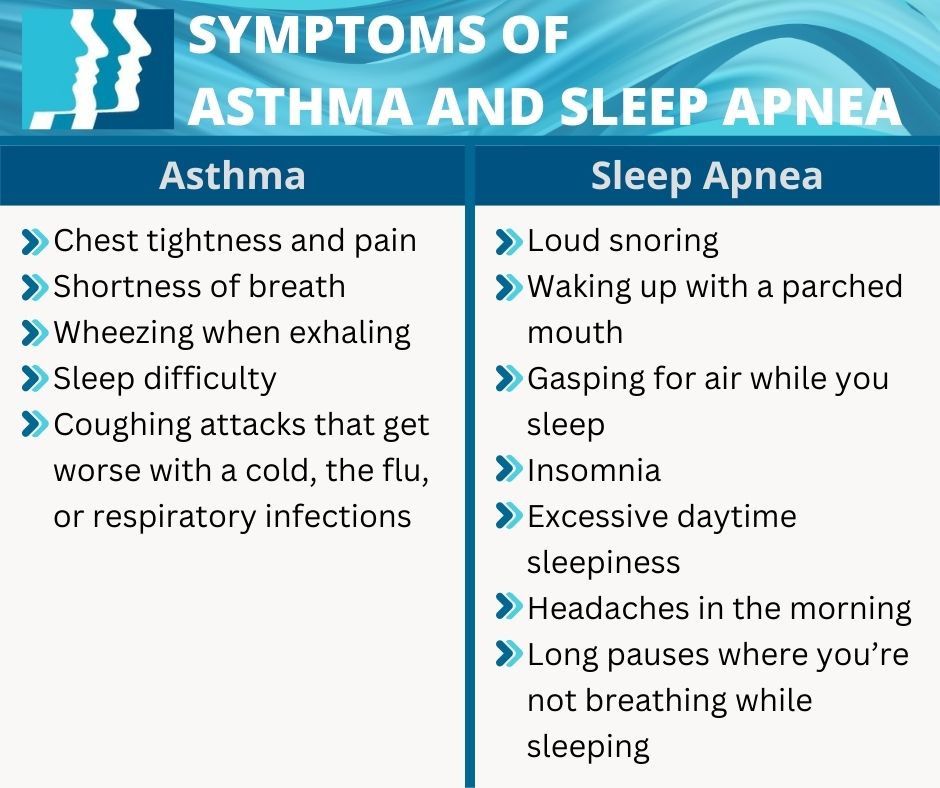
Asthma symptoms can vary from person to person, but they often include:
- Chest tightness and pain
- Shortness of breath
- Wheezing when exhaling
- Sleep difficulty
- Coughing attacks that get worse with a cold, the flu, or respiratory infections
Unfortunately, there’s no “cure” for asthma, but an individualized treatment plan incorporating medications, medical monitoring, and lifestyle changes can help manage it.
What is Sleep Apnea?
Sleep apnea is a sleep disorder in which breathing repeatedly starts and stops during sleep. Unlike asthma, which is a narrowing of the airways within the lungs themselves, sleep apnea is a physical obstruction of the airways before air reaches the lungs.
Usually, the physical blockage, which can be by the tongue, the tonsils, or one’s own body weight, occurs above the trachea, aka the windpipe.
There are three main types of sleep apnea:
- Obstructive sleep apnea is the most common type of sleep apnea, which occurs when the throat muscles relax too much during sleep.
- Central sleep apnea happens when your brain doesn’t send proper messages to the muscles that control breathing.
- Complex sleep apnea syndrome occurs if you have both obstructive sleep apnea and central sleep apnea.
Common signs and symptoms of sleep apnea include:
- Loud snoring
- Waking up with a parched mouth
- Gasping for air while you sleep
- Insomnia
- Excessive daytime sleepiness
- Headaches in the morning
- Long pauses where you’re not breathing while sleeping (reported by someone else)
What Are the Treatment Options for Asthma and Sleep Apnea?
Thankfully, both asthma and obstructive sleep apnea have a variety of treatment options.
Treatment Options for Asthma
For asthma, there’s an increasing spectrum of treatment options from minimal to maximal. These include:
- A rescue inhaler, a small, handheld device that pumps medication into your mouth and down to your lungs. The medicine opens your airways so you can breathe easier. Some people with mild asthma may only need to use an inhaler every once in a while. If you find yourself using a rescue inhaler more than twice a week, you probably need more long-term treatment.
- Inhaled steroids or bronchodilators are like inhalers, but they are long-acting and are used to control asthma symptoms instead of just providing quick, short-term relief. The steroids work to treat asthma by reducing inflammation in the lungs.
- A combination of treatments may be necessary if you have very severe asthma. A doctor might have you use a rescue inhaler, bronchodilator, and oral steroids together to control and relieve your asthma symptoms.
- Injectable medications for asthma are also sometimes necessary for severe asthma. These medications are in a class of drugs called monoclonal antibodies, which block the response to airway triggers that cause inflammation. People with severe asthma typically receive this type of treatment every 2–8 weeks, and it may be administered at a doctor’s office, hospital, or via self-injection at home.
Treatment Options for Sleep Apnea
For those with sleep apnea, treatment options include:
- Continuous positive airway pressure (CPAP) therapy, which is a machine with a hose that connects to a mask. The hose delivers constant and steady oxygen while you sleep. Unfortunately, some people have problems with leaky masks, insomnia, dry mouth, and/or other issues related to CPAP, and should consider CPAP alternatives in those cases.
- Weight loss can help treat sleep apnea by reducing fat deposits in your neck and tongue to improve airflow while you’re sleeping.
- Surgery is another alternative treatment for sleep apnea and may include a tonsillectomy (removal of the tonsils), nasal surgery, or Inspire (hypoglossal nerve stimulator surgery). Inspire is a tiny, implanted device that controls your breathing by sending a small electrical signal to the nerve that controls your tongue. Once it’s implanted, you use a small handheld remote to turn it on before bed and off when you wake up. Unlike CPAP, there’s no hose or mask needed.
When Is It Time to See a Doctor?
Asthma and sleep apnea are severe conditions that require ongoing treatment and medical monitoring. If you’re experiencing symptoms of either condition, such as shortness of breath, difficulty breathing, loud snoring, or you stop breathing intermittently overnight, see a doctor immediately.
Here at ENT Associates of Lubbock, we’re eager to help you address your asthma and sleep apnea with a treatment method that’s tailored to you.
Dr. Cuthbertson is a physician at Ear Nose & Throat Associates of Lubbock. He joined the team at ENT Lubbock from Houston, where he was chief resident of the prestigious Bobby R. Alford Department of Otolaryngology at Baylor College of Medicine. He is board certified in Otolaryngology and Head & Neck Surgery and has quickly built a reputation, not only as an extremely skilled surgeon, but as an approachable and compassionate clinician adept in the newest standards and technologies. Learn more about Dr. Cuthbertson.
Categories: