Everyone knows what it’s like to wake up feeling a little run down or with a runny nose, congestion, or cough.
A few years ago, you’d just assume you had a cold and move on with your life. If you’re an allergy sufferer, you’d pop a Zyrtec and head to the office. A fever would cause a little more trouble; you might take it easy for a bit and then everything would return to normal.
Today, things are a little different.
COVID is on everyone’s mind. Symptoms that wouldn’t have caused a second thought before are now cause for anxiety. What’s that tickle in your throat? Why are you coughing? Is this runny nose really from your ragweed allergy, or is it COVID?
Unfortunately, during surges in COVID case numbers, you’re not being paranoid — a high level of suspicion is necessary.
In this post, we want to help you understand the likelihood of your symptoms being COVID versus something else like allergies, the flu, or a cold.
Allergies or COVID?
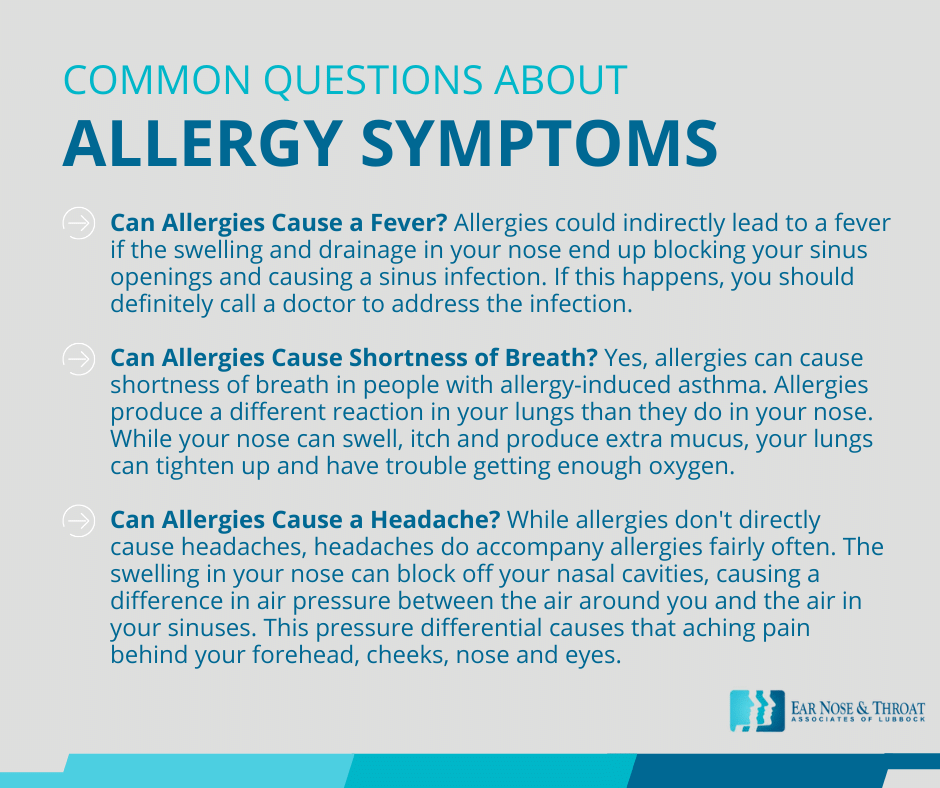
Allergies are an overreaction of the immune system to a relatively harmless environmental stimulus. Histamine, one of the body’s chemical messengers, works to fight off these perceived threats as quickly as possible. The histamine reaction causes swelling, sneezing, tearing of the eyes, and itching.
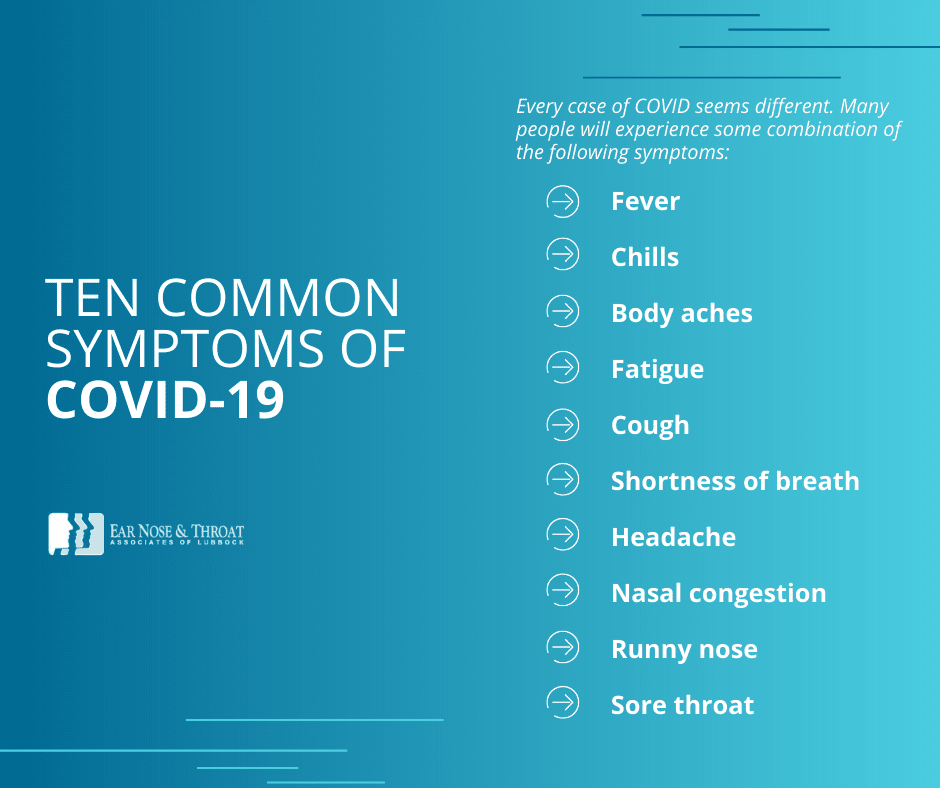
Allergies and COVID share a few similar symptoms, like a headache and runny nose. But COVID often comes with whole-body symptoms like a fever, chills, body aches, cough, and exhaustion.
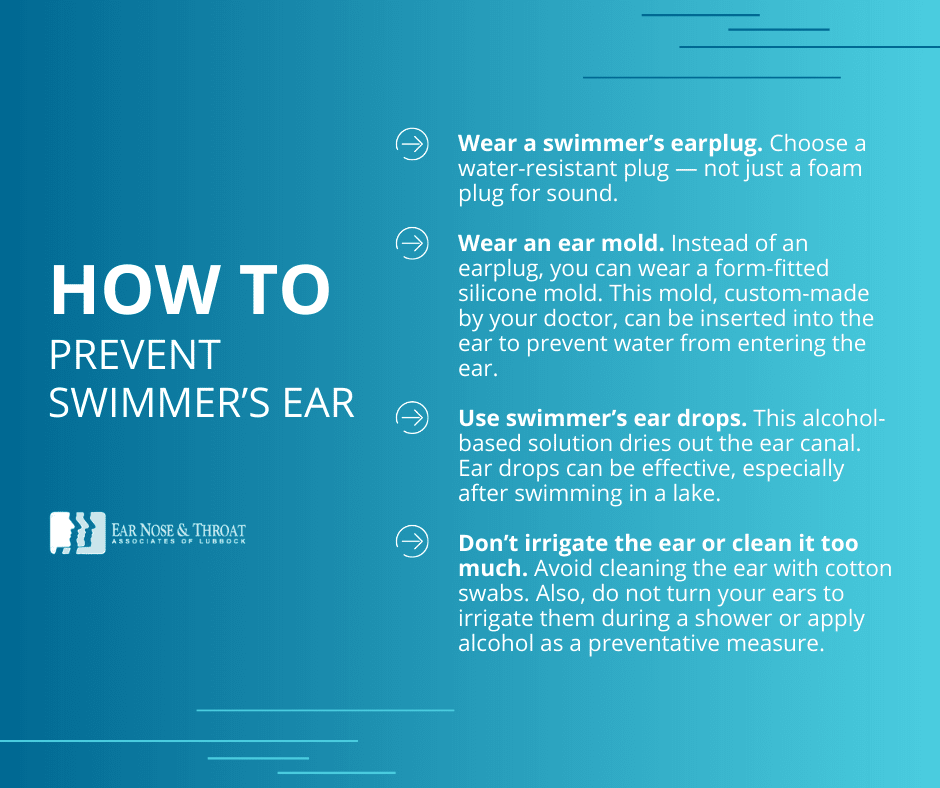
Allergy symptoms, caused by histamine reactions, tend to be concentrated in the upper respiratory system. Sneezing, congestion, runny nose, and itchy, watery eyes are all hallmark signs of allergies. And while allergies occasionally cause a cough, it’s not generally the nagging, persistent cough that can accompany COVID.
Taking an over-the-counter antihistamine is one of the best ways to determine whether you’re dealing with COVID or allergies. An antihistamine (such as Claritin, Zyrtec, Allegra, or Xyzal) won’t help with COVID, but it should help improve allergy symptoms.
A Common Cold or COVID?
A variety of viruses can cause the common cold: rhinoviruses, RSV, parainfluenza, and coronaviruses. COVID, however, is caused by a specific coronavirus called SARS-CoV-2.
Early in the pandemic, symptoms of the common cold were somewhat easier to distinguish from COVID. But COVID has changed over time and now has several variants. Omicron, for example, has a somewhat milder presentation, making it difficult to distinguish from a cold based on symptoms alone. Both illnesses can present with nasal congestion, runny nose, and sore throat, but in our office we’ve noticed that some patients with Omicron don’t have the fever or cough that people have had with other COVID variants.
“Better safe than sorry” is the motto here. If you find yourself with symptoms of the common cold, go ahead and get tested — especially if you know you’ve been exposed to someone who has COVID. During a surge in COVID cases, it’s reasonable to assume you’re dealing with COVID until you’re shown otherwise.
Influenza or COVID?
Mild cases of COVID closely mimicked influenza (“the flu”) during the beginning of the pandemic. And it can still be difficult to tell the difference between the symptoms.
The flu typically involves a fever, body aches, chills, cough, congestion, and a headache. But COVID, especially the earlier variants, usually involves most of these symptoms too! A loss of taste and smell is the hallmark symptom that often differentiates between these two infections.
Again, the safest course of action if you’re experiencing flu-like symptoms is to get tested. Many doctors’ offices and other facilities offer rapid flu tests along with COVID tests, so you can know for sure whether you have one or the other. Several effective antiviral medications exist for the flu — good news if you receive a positive flu test!
A Note About the Loss of Taste and Smell
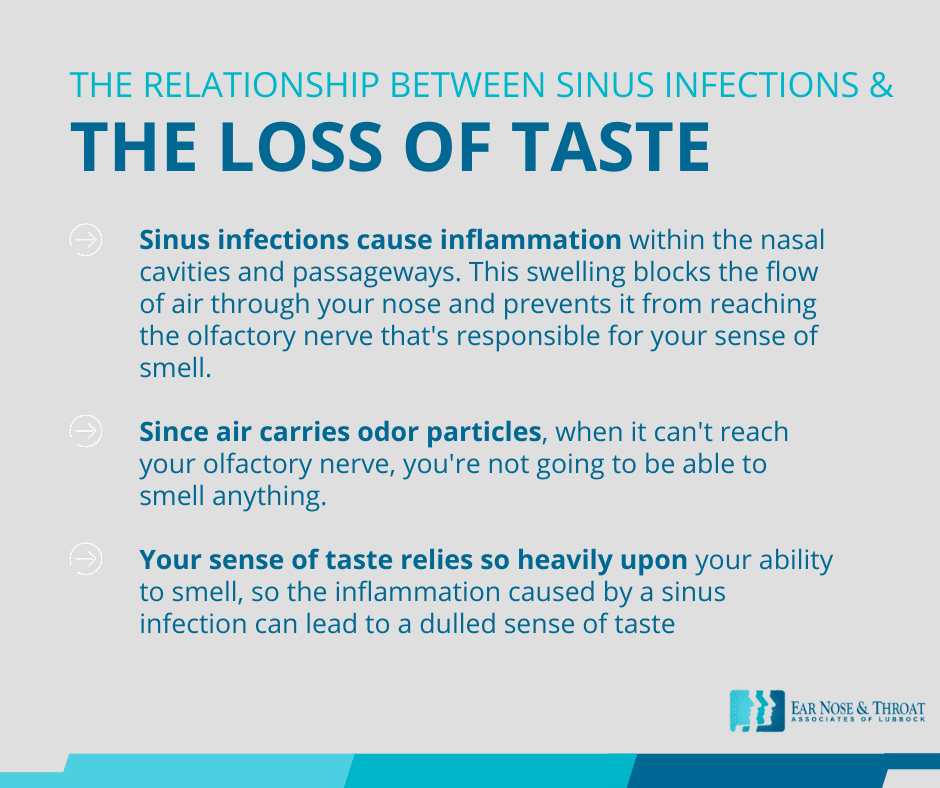
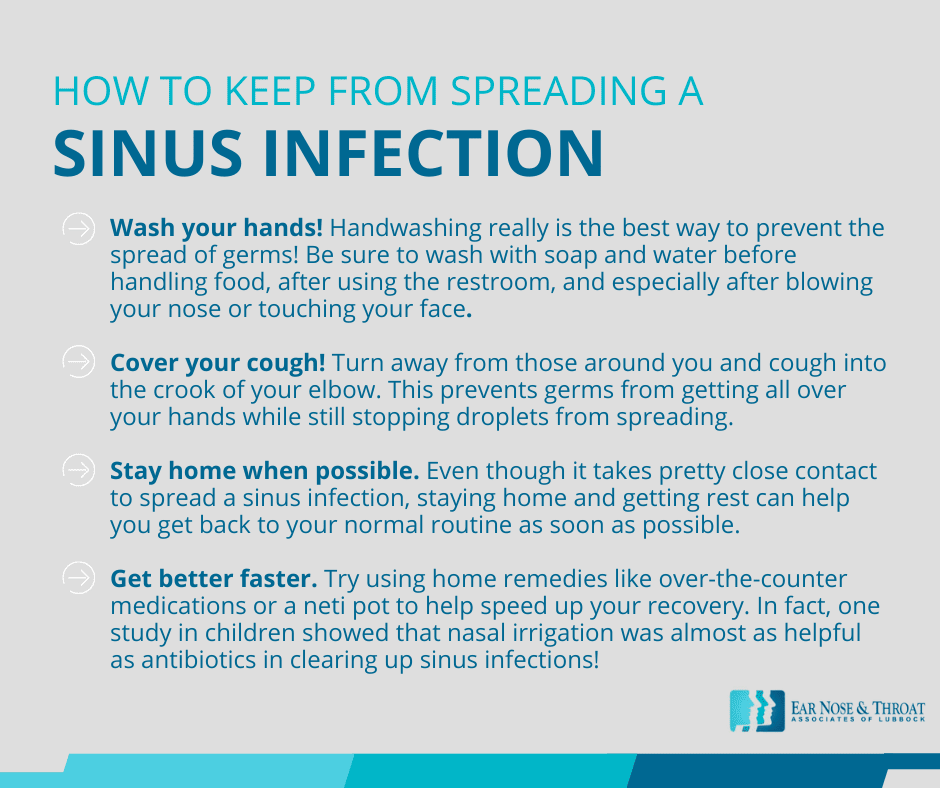
One final note about all of these conditions: You probably know that loss of taste and smell is a classic sign of COVID. But occasionally during allergies, a cold, or the flu, the sinuses become blocked by mucus or swelling, leading to a sinus infection. This swelling can block the airflow through your nose, preventing it from reaching the olfactory nerve that’s responsible for your sense of smell.
Since odor particles are carried in the air, you won’t be able to smell anything when air can’t reach your olfactory nerve. And because your ability to taste relies so heavily upon your sense of smell, a sinus infection can lead to a loss of sense of taste as well. Because of this, a COVID test really is the best way to tell the difference.
Do I Have COVID-19?
In the end, you should err on the side of caution (particularly during COVID surges). Unfortunately, the only way to completely rule out a case of COVID is to get tested and wait for the results.
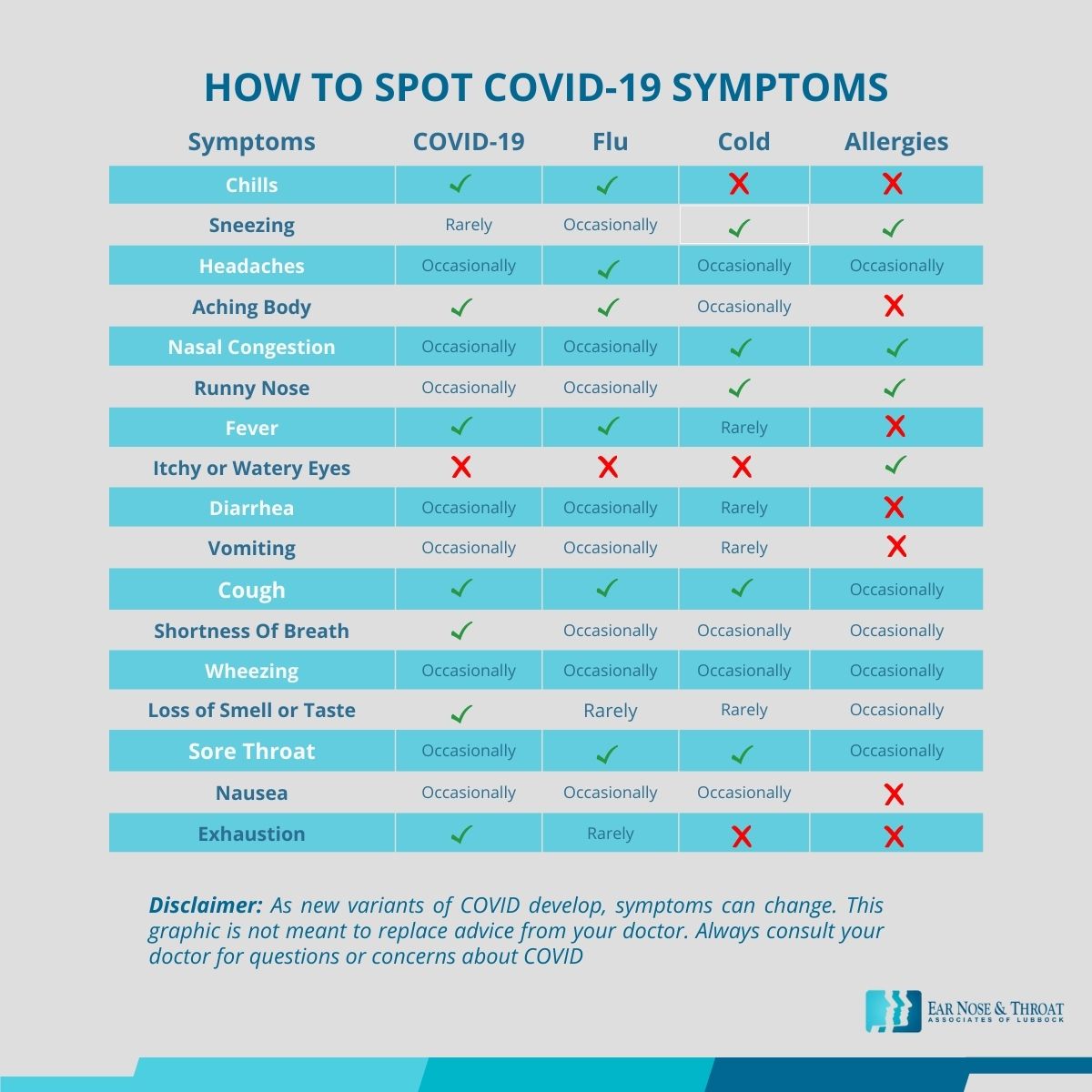
We’ve included a chart with the common symptoms of COVID-19, the flu, a common cold, and allergies in this post for your reference. But keep in mind that as new COVID variants develop, symptoms can change, and COVID symptoms vary widely from person to person.
If you have questions about whether your symptoms are COVID, allergies, or something else, we recommend consulting with your doctor and scheduling a COVID test. You can also always refer to the current Centers for Disease Control and Prevention (CDC) COVID guidelines.
Dr. Cuthbertson is a physician at Ear Nose & Throat Associates of Lubbock. He joined the team at ENT Lubbock from Houston, where he was chief resident of the prestigious Bobby R. Alford Department of Otolaryngology at Baylor College of Medicine. He is board certified in Otolaryngology and Head & Neck Surgery and has quickly built a reputation, not only as an extremely skilled surgeon, but as an approachable and compassionate clinician adept in the newest standards and technologies. Learn more about Dr. Cuthbertson.