Hearing. It’s one of the senses we rely heavily upon to understand our world. And like most of our five senses, we never seem to fully appreciate it until it’s gone.
Though not all hearing loss is preventable, much of it is. And the good news is that taking a few simple measures will minimize your chances of hearing impairment.
Below, we’ll look at how to prevent hearing loss and five steps you can take to protect your hearing.
Why Is Preventing Hearing Loss So Important?
As an ENT doctor, I typically see two main contributing factors of hearing loss in my practice: genetics and noise.
We inherit genetic hearing loss from our families, and unfortunately, there’s not much we can do to prevent that. People with genetic hearing loss can be careful to protect their hearing their whole lives and still wind up unable to hear in their later years.
But noise-induced hearing loss can be prevented.
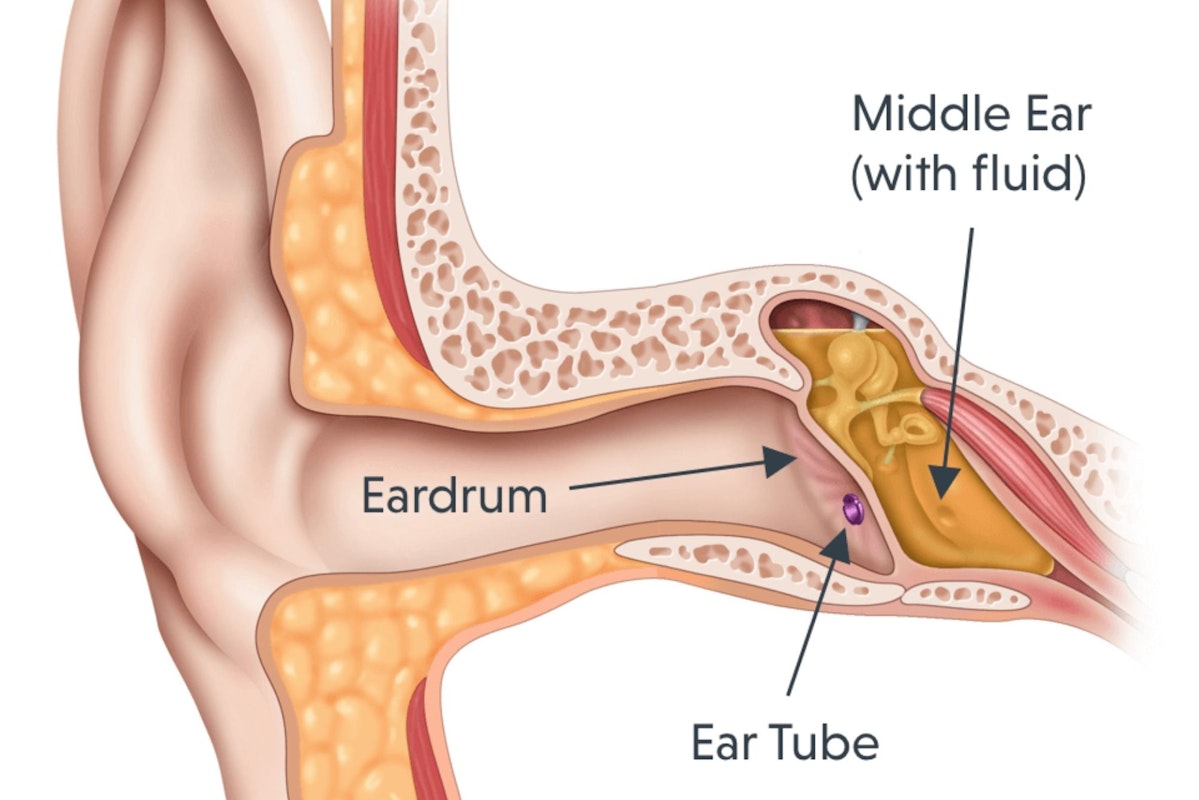
Noise-induced hearing loss occurs because we’re exposed to sounds that are just too loud for us. Deep in our inner ears, sound waves activate tiny hair-like cells that then send signals our brain interpret as sound. Too much sound, though, damages these little hairs, and they never heal or recover.
This is noise-induced hearing loss.
We often see noise-induced hearing loss in farmers and oil field workers who spend their days working around heavy machinery. Anyone who spends much time in front of blasting speakers or shooting guns without ear protection will likely develop hearing loss as well.
The trouble is, we don’t think about hearing loss when we’re young; we think we’re invincible. By the time we realize the need for hearing protection, sometimes the damage is already done. And because those little hair cells never heal, the only course of action at this point is hearing aids.
Perhaps because of these risk factors, men between the ages of 20 and 69 are almost twice as likely to develop hearing loss as their female counterparts. And more than a billion young adults are at risk of permanent, yet preventable, hearing loss due to unsafe listening practices.
The good news is that once you know what causes the damage, you’re well on your way to understanding how to prevent hearing loss.
How To Prevent Hearing Loss
Here are five of the most important steps you can take to prevent hearing loss. By following these, you will significantly decrease your risk of noise-induced hearing damage.
Tip #1: Always Wear Hearing Protection Around Loud Noises
You may not think you need hearing protection, but you might be surprised what levels of sound can harm your ears.
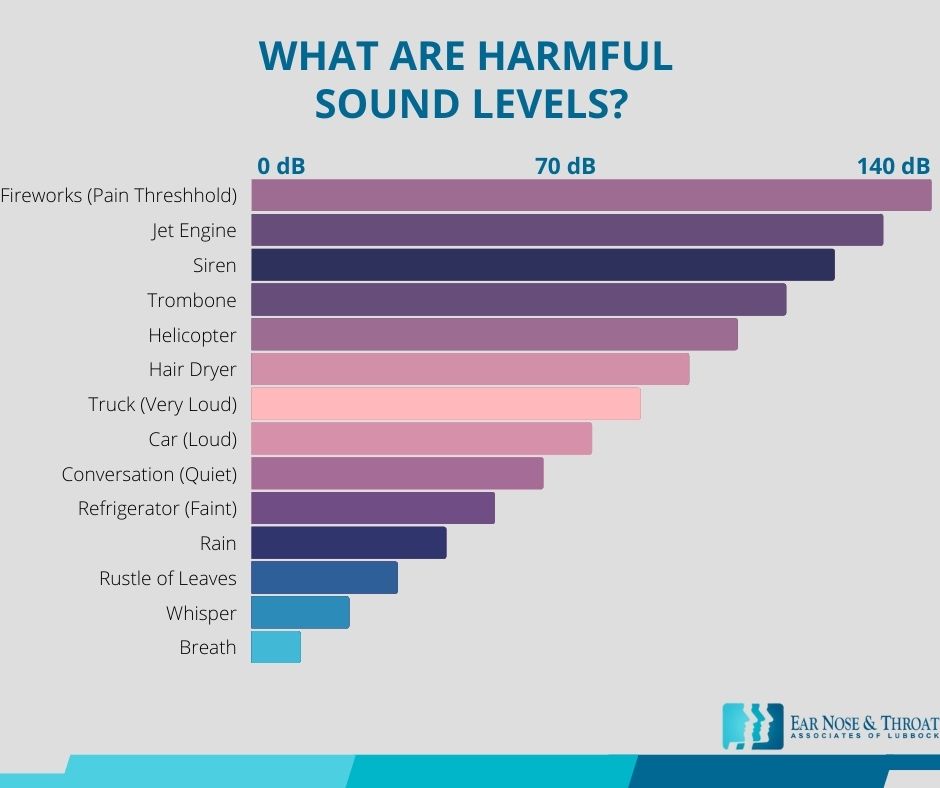
The Centers for Disease Control (CDC) and the World Health Organization (WHO) note that prolonged exposure to noise over 70 decibels (dB) or hour-long exposure to noise at 85 dB can cause hearing loss. Noise at 110 dB can cause permanent hearing loss in less than two minutes, and 120 dB and above can cause immediate damage.
For some context, normal speaking volume is around 60 dB, and a loud vacuum cleaner or hair dryer is about 70–75 dB. A hand saw, blender, or noisy restaurant produces around 85 dB, and thunderclaps, ambulance sirens, and pneumatic drills reach 120 dB.
Jet engines, gunshots, and stock car races all well exceed 120 dB.
So whether you attend a concert or work with heavy machinery, power tools, or construction equipment, if the sound might exceed a safe decibel level, you should wear hearing protection.
Even if you’re attending an acoustic or classical music concert, bringing hearing protection along with you is a good idea in case you find yourself sitting in front of a speaker.
Both ear plugs and over-the-ear muffs can provide effective hearing protection.
Ear plugs generally block more noise because they fill up the ear canal to block sound waves from entering. Plugs are also more effective for preventing damage from low-frequency noises; think diesel engines, compressors, wind turbines, and thunder.
Ear plugs are also less conspicuous than ear muffs, which many people find appealing.
Over-the-ear muffs, on the other hand, are more effective at protecting your hearing from high-frequency noises; think whistles, motorcycles, turbochargers, and crashing cymbals.
Ear plugs alone can cut noise levels by 30 dB, but wearing both in-the-ear and over-the-ear protection together can provide the best protection if you’re in a particularly loud environment, like a gun range or machinery-heavy workplace.
Tip #2: Make Sure Your Hearing Protection Fits Properly
Wearing ear protection in noisy environments is a great start. But hearing protection can’t help if it doesn’t fit properly!
Ear plugs should fit snugly inside the ear with no gaps or movement. You may need to try out a few brands and sizes to find the ear plugs that fit you best.
Hearing protection ear muffs should fit snugly over the entire outside of the ear. And if you’re going to be exposed to noise levels over 105 dB for a prolonged period, it’s best to wear both ear plugs and ear muffs together.
Tip #3: Understand How Decibels Are Measured
Even if we know that decibels measure sound intensity, the decibel scale can be confusing.
It’s important to remember that decibels are measured on a logarithmic scale, not a linear one. This means each decibel increase indicates an exponentially louder sound.
Normal breathing, for example, is about 10 dB, and a ticking watch registers around 20 dB. This doesn’t mean that a watch is twice as loud as breathing, but that it’s 10 times louder than breathing.
So a few more decibels in sound aren’t quite as harmless as you might think.
Tip #4: Take a Break During Prolonged Exposure to Loud Noises
If you need to be around loud noises for a long period of time, try to take some breaks. Even if the noise doesn’t seem that loud, prolonged exposure to excess noise causes damage to hearing.
The Occupational Safety and Health Administration (OSHA) sets permissible exposure limits, or PELs, for the noise exposure allowed in workplaces. They permit a full eight-hour workday at 90 dB, for example, but for every 5 dB increase, they cut the time in half.
Tip #5: Keep Noises at Reasonable Levels
Many of us like to have constant noise with us as we go about our day. We crank up the radio and belt out a tune during our commute. We listen to podcasts while we go for a walk or cook dinner for the family. The noise of the television keeps us company in the evenings.
But in our zeal to listen to our favorite tunes and catch up on our favorite podcasts, it’s easy to get carried away. Most smartphones have apps that can measure decibels, and the iPhone even warns you if your volume is approaching dangerous levels.
You don’t need to strain to hear your favorite song, but try to keep the volume at a reasonable level. Your future self will thank you!
Protect Your Hearing and Get Tested if You’re Concerned
Maybe you work in a noisy car wash, frequent Nascar races, or enjoyed a stint as a punk rock groupie. Or maybe you hit the shooting range to unwind on the weekends. Whatever your pastimes, we hope you’ll employ these tips to prevent hearing loss.
If you have any concerns about your hearing — like ringing in your ears or not being able to understand people’s words — you can always schedule a hearing test with an ENT doctor or board-certified audiologist.
They can assess your current level of hearing and keep you listening to the world around you as long as possible!
Dr. Cuthbertson is a physician at Ear Nose & Throat Associates of Lubbock. He joined the team at ENT Lubbock from Houston, where he was chief resident of the prestigious Bobby R. Alford Department of Otolaryngology at Baylor College of Medicine. He is board certified in Otolaryngology and Head & Neck Surgery and has quickly built a reputation, not only as an extremely skilled surgeon, but as an approachable and compassionate clinician adept in the newest standards and technologies. Learn more about Dr. Cuthbertson.
Dr. Scolaro is a board-certified Otolaryngologist servicing the South Plains area. He has been practicing in Lubbock since 1990 and has earned a reputation as a skilled and experienced surgeon. He currently serves as the Medical Director for Covenant High Plains Surgery Center campuses, is a member of Covenant Health Partners and is an adjunct faculty professor for Texas Tech University Health Sciences Center School of Medicine. Learn more about Dr. Scolaro.